
Pain in the pelvis
Pain in the pelvis. Pain in the pelvis can often be linked to pregnancy or miscarriage over a long period of time. Pain in the pelvis is a problem that affects up to 50% of pregnant women according to the large Norwegian mother / child survey (also known as MoBa). Pain in the pelvis and nearby structures such as the lower back and hip is of course not a unique problem for pregnant women or those who have recently given birth - muscular or joint dysfunction can affect both women and men, young and old.
Scroll below to see two great exercise videos that can help you with pelvic pain and tight glutes.
VIDEO: 5 Exercises against Sciatica and Sciatica
In the pelvis and seat we also find the sciatica nerve. This nerve tends to become irritated and pinched by pelvic problems - and this can cause episodic sharp, almost stabbing pains in the seat. Here are five exercises that can relieve nerve pain and provide better pelvic function. We recommend that you do these daily if you have pelvic problems.
Join our family and subscribe to our YouTube channel for free exercise tips, exercise programs and health knowledge. Welcome!
VIDEO: 5 Strength Exercises Against Back Prolapse
In the case of pelvic problems it is also important to strengthen the deep back muscles - so you can relieve your overloaded pelvis. Precisely for this reason, we have chosen these gentle and adapted strength exercises that can also be used even if you have a back prolapse. Click below to see them.
Did you enjoy the videos? If you took advantage of them, we would really appreciate you subscribing to our YouTube channel and giving us a thumbs up on social media. It means a lot to us. Thank you very much!
Common causes and diagnoses of pelvic pain:
- Atrosis / osteoarthritis (the pain depends on which joints are affected)
- Pelvic (the wound is often located in the lumbosacral / hip region, and has associated myoses in glutes musculature)
- pelvic locker (typically causes pain and dysfunction of the iliosacral joints, as well as the lower back)
- Gluteus maximus myalgia / trigger point (causes typical myosis pain in the seat, tailbone and occasional ileing in the back of the thigh)
- Gluteus medius myalgia / trigger point (can cause deep pain in the seat and the transition to the lower back, can also contribute to false sciatica)
- Gluteus minimus myalgia / trigger point (may cause deep pain in the seat and occasional tingling all the way down to the outside of the lower leg)
- Ischiogluteal bursitis (gluteal mucositis) (may cause severe pain, reddish swelling and inflammation-like pain in the buttock region)
- Obturator internus myalgia / trigger point (myosis that can refer pain deep to the tailbone, hip and glutes)
- rheumatism (the pain depends on which joints are affected)
The Norwegian Mother and Child Survey (MoBa)
The MoBa survey was conducted in the years 1999-2008. Over 90000 pregnant women participated in the survey. In this study, almost half stated that they had had pain in one or more stages of pregnancy. 15% reported that they had pelvic floor syndrome in the latter part of pregnancy.
Also read: Hit by Sciatica in Or After Pregnancy? Try these 5 Exercises Against Sciatica
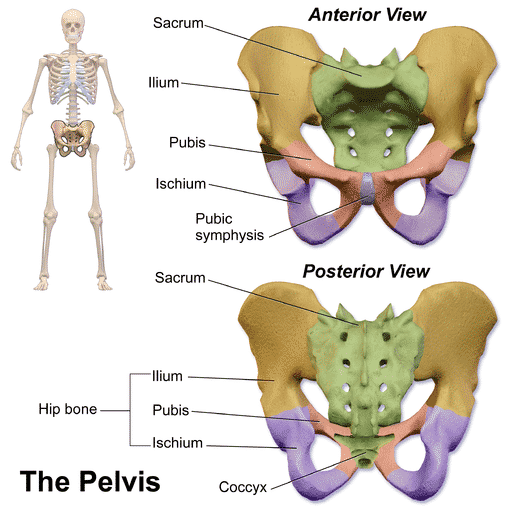
Anatomy of the pelvis
What we call the pelvis, also known as pelvis (ref: large medical lexicon), consists of three parts; pubic symphysis, as well as two iliosacral joints (often called pelvic joints). These are supported by very strong ligaments, which give the pelvis a high load capacity. In the SPD (symphysis pubic dysfunction) report from 2004, obstetrician Malcolm Griffiths writes that none of these three joints can move independently of the other two - in other words, movement in one of the joints will always result in a counter movement from the other two joints.
If uneven movement occurs in these three joints, we can get a combined joint and muscular problem. This can become so problematic that it will require musculoskeletal treatment to correct it, e.g. physiotherapy, chiropractic or manual therapy.
X-ray of female pelvis
In the x-ray above you can see a female pelvis / pelvis (AP view, front view), consisting of sacrum, ilium, iliosacral joint, tailbone, symphysis etc.
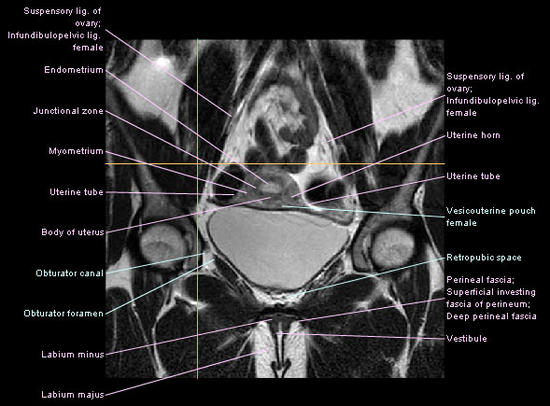
MRI image / examination of female pelvis
In the MR image / examination above you see a female pelvis in a so-called coronal cross-section. In MRI examination, versus X-ray, soft tissue structures are also visualized in a good way.
Causes
Some of the most common causes of such ailments are natural changes throughout pregnancy (changes in posture, gait, and change in muscular load), sudden overloads, repeated failure over time, and little physical activity. Often it is a combination of causes that cause pelvic pain, so it is important to treat the problem in a holistic way, taking into account all factors; muscles, joints, movement patterns and possible ergonomic fit.
Pelvic
Pelvic dissection is one of the very first things that is mentioned when it comes to pelvic pain. Sometimes it is mentioned correctly, other times by mistake or lack of knowledge. Relaxin is a hormone found in both pregnant and non-pregnant women. During pregnancy, relaxin works by producing and remodeling collagen, which in turn leads to increased elasticity in muscles, tendons, ligaments and the tissue in the birth canal - this provides enough movement in the involved area for the child to be born.
But, and it's a big but. Research in several large studies has ruled out that relaxin levels are a cause of pelvic joint syndrome (Petersen 1994, Hansen 1996, Albert 1997, Björklund 2000). These relaxin levels were the same in both pregnant women with pelvic joint syndrome and those without. Which in turn leads us to the conclusion that pelvic joint syndrome is a multifactorial problem, and should be treated accordingly with a combination of training aimed at muscle weaknesses, joint treatment and muscle work.
- Also read: Why did I have so much back pain after pregnancy?
pelvic locker
Pelvic locking is another term that is also frequently used. It indicates that the iliosacral joints have a dysfunction / reduced movement, and as shown in Griffiths' SPD report (2004), we know that if we have a joint that does not move then this will affect the other two joints that make up the pelvis. The iliosacral joints have very small range of motion, but the joints are so essential that even minor restrictions can cause dysfunction in nearby muscles or joints (e.g. lower back or hip).
The link to the lumbar spine is obvious if we think from a biomechanical point of view – the lower vertebrae are the closest neighbors to the iliosacral joints and can be affected by musculoskeletal problems in the pelvis. This is illustrated by the fact that joint therapy aimed at both the lower back and the pelvis is more effective than only joint therapy aimed at the pelvic joint, as shown in a recent study in the Journal of Bodywork and Movement Therapies.
In the study, they examined two different manual adjustments (as performed by chiropractors and manual therapists) and compared their effect on patients with sacroiliac joint dysfunction - also known as pelvic joint dysfunction, pelvic lock, ileosacral dysfunction or pelvic joint lock in the vernacular and vernacular.
The study (Shokri et al, 2012), a randomized controlled trial, wanted to clarify the difference between adjusting only the pelvic joint compared to adjusting both the pelvic joint and the lumbar spine, in the treatment of pelvic joint locking.
To jump straight to the nitty-gritty, the conclusion was as follows:
… «A single session of SIJ and lumbar manipulation was more effective for improving functional disability than SIJ manipulation alone in patients with SIJ syndrome. Spinal HVLA manipulation may be a beneficial addition to treatment for patients with SIJ syndrome. » …
It thus appeared that adjusting both the pelvic joint and the lumbar spine was significantly more effective when it came to pain relief and functional improvement in patients who had been diagnosed with pelvic joint dysfunction.
Classification of pelvic pain.
Pain in the pelvis can be divided into acute, subacute and chronic pain. Acute pelvic pain means that the person has had pain in the pelvis for less than three weeks, subacute is the period from three weeks to three months and the pain that has a duration of more than three months is classified as chronic. Pain in the pelvis can be caused by muscular tension, joint dysfunction and/or irritation of nearby nerves. A chiropractor or another expert in muscle, bone and nerve disorders can diagnose your condition and give you a thorough explanation of what can be done in terms of treatment and what you can do on your own. Make sure you don't walk with pelvic pain for a long time, rather contact a chiropractor (or other musculoskeletal expert) and get the cause of the pain diagnosed. When you know the cause, it becomes much easier to do something about it.
Clinically proven effect on pelvic and lower back pain relief.
- A recent RCT showed that joint treatment of both pelvic joints and lumbar spine was more effective in the treatment of pelvic joint syndrome (Kamali, Shokri et al, 2012)
- A systematic review of studies, a so-called meta-study, concluded that chiropractic manipulation is effective in the treatment of subacute and chronic low back pain (Chou et al, 2007).
What does a chiropractor do?
Muscle, joint and nerve pain: These are things that a chiropractor can help prevent and treat. Chiropractic treatment is mainly about restoring movement and joint function that can be impaired by mechanical pain. This is done by so-called joint correction or manipulation techniques, as well as joint mobilization, stretching techniques, and muscular work (such as trigger point therapy and deep soft tissue work) on the involved muscles. With increased function and less pain, it may be easier for individuals to engage in physical activity, which in turn will have a positive effect on both energy and health.
Exercises, training and ergonomic considerations.
Based on your diagnosis, an expert in musculoskeletal disorders can inform you of the ergonomic considerations you must take to prevent further damage, and thus ensure the fastest possible healing time. After the acute part of the problem is over, you will also in most cases be assigned specific home exercises that also help to reduce the chance of recurrence. In the case of chronic ailments, it is necessary to go through the motor movements you do in everyday life, in order to weed out the reason why your pain occurs again and again. It is important that any training program has a gradual build-up / progression - otherwise you risk getting strain.
What can you do yourself?
1. General exercise, specific exercise, stretching and activity are recommended, but stay within the pain limit. Two walks a day of 20-40 minutes make good for the body and aching muscles.
2. Trigger point / massage balls we strongly recommend - they come in different sizes so you can hit well even on all parts of the body. There is no better self help than this! We recommend the following (click the image below) - which is a complete set of 5 trigger point / massage balls in different sizes:
3. Training: Specific training with training tricks of various opponents (such as this complete set of 6 knits of different resistance) can help you train strength and function. Knit training often involves more specific training, which in turn can lead to more effective injury prevention and pain reduction.
4. Pain Relief - Cooling: Biofreeze is a natural product that can relieve pain by cooling the area gently. Cooling is especially recommended when the pain is very severe. When they have calmed down then heat treatment is recommended - it is therefore advisable to have both cooling and heating available.
5. Pain Relief - Heating: Warming up tight muscles can increase blood circulation and reduce pain. We recommend the following reusable hot / cold gasket (click here to read more about it) - which can be used both for cooling (can be frozen) and for heating (can be heated in the microwave).
- Here you will find an overview and list of exercises we have published in connection with the prevention, prevention and relief of pelvic pain, pelvic pain, pelvic locking, osteoarthritis and other relevant diagnoses.
Overview - Exercise and exercises for pelvic pain and pelvic pain:
5 Good Exercises Against Sciatica
6 strength exercises for stronger hips
Recommended products for effective training of the pelvis and hip (see knitting exercises on the product page):
Read more: Complete Set of 6x Mini-Bands
Difficulty finding a good lying position? Tried ergonomic pelvic pillow?
Some think that a so-called pelvic pad can provide good relief for back pain and pelvic pain. Press here or on the image above to read more about this.
Research and references:
- SPD: The Clinical Presentation, Prevalence, Aetiology, Risk Factors and Morbidity. Malcolm Griffiths.
- Normal Serum Relaxin in Women with Disabling Pelvic Pain During Pregnancy. Gynecol Obstet Invest. 1994; 38 (1): 21-3, Petersen LK, Hvidman L, Uldbjerg N
- Symphyseal Distention in Relation to Serum Relaxin Levels and Pelvic Pain in Pregnancy. Acta Obstet Gynecol Scand. 2000 Apr; 79 (4): 269-75. Björklund K, Bergström S, Nordström ML, Ulmsten U
- Relaxin is not related to symptom-giving pelvic girdle relaxation in pregnant women. Acta Obstet Gynecol Scand. 1996 Mar; 75 (3): 245-9. Hansen A, Jensen DV, Larsen E, Wilken-Jensen C, Petersen LK.
- Circulating levels of relaxin are normal in pregnant women with pelvic pain. Eur J Obstet Gynecol Reprod Biol. 1997 Jul; 74 (1): 19-22. Albert H, Godskesen M, Westergaard JG, Chard T, Gunn L.
- Kamali & Shokri (2012). The effect of two manipulative therapy techniques and their outcome in patients with sacroiliac joint syndrome. Journal of Bodywork and Movement TherapiesVolume 16, Issue 1, January 2012, Pages 29–35.
 Follow Vondt.net on YOUTUBE
Follow Vondt.net on YOUTUBE
(Follow and comment if you want us to make a video with specific exercises or elaborations for exactly YOUR issues)
 Follow Vondt.net on FACEBOOK
Follow Vondt.net on FACEBOOK
(We try to respond to all messages and questions within 24-48 hours)












Hi all. Need some tips. Was born with a crooked pelvis and has been bothered a lot with the pelvis, hip and back all his life (is 29). Was at the physio already when I was 15 years old, was then told that I had a very crooked pelvis and that this made everything crooked (naturally enough) in the body. Finished treatment with her, but never went to further treatment. Had 4 children, first 10 years ago. And has gradually only gotten worse and worse. Have arthritis, rheumatism and ankylosing spondylitis in the family, and in recent years I have bitten my teeth together due to pain in the hip (especially on the right side) and have told myself that it will probably pass. I have managed with Paracet and Ibux at times, but now that the cold has hit I have really felt it. Is inflamed on the entire outside of the hip, and has continuous pain. Can mention that when I am out walking, my hips "stiffen" after a while and I start to limp. Have had an appointment for an X-ray next month, but think it is a very long time to wait with so much pain, so consider calling the doctor to get another appointment, there must be something anti-inflammatory I can get outside of Ibux? I dread X-rays when I fear osteoarthritis changes.
Someone who recognizes himself?
Hey!
Hope someone might be able to answer a question .. I know everything is individual, but maybe someone has similar experiences?
Some background:
I have been diagnosed with fibromyalgia for almost 7 years now. Has Norspan patch with 10 micrograms strength. The doctor describes it as "strong type of fibromyalgia".
Impacts mostly on joints in fingers, wrists, ankles and toes, back / pelvis and fatigue even how much / little I sleep. Can not stretch my fingers now when it is cold, and all of the strength in the body is gone and pretty much everything is painful.
Apart from sc, I have 3 prolapses in the back and 2 in the neck, have a spondylolisthesis, have congenital rotation in the pelvis and mild scoliosis.
So to the question:
In the last couple of weeks / months I have had problems with one knee, where it feels like half the knee is asleep and failing. Have any of you been away in the same? Does it have a connection with FM? Possibly with rotation in the pelvis? Am I in the middle of an aggravation? Or is it something else?